Drug interactions, particularly with prescription medications, are complex occurrences where substances, including food, beverages, or other drugs, can lead to pharmacokinetic changes. These alterations can significantly affect a medication’s intended function, potentially resulting in detrimental consequences. One widely recognized example involves grapefruit juice, which can diminish the effectiveness of certain medications. Additionally, although not classified as a drug itself, activated charcoal has a well-documented ability to interfere with or entirely nullify the effects of numerous medications.
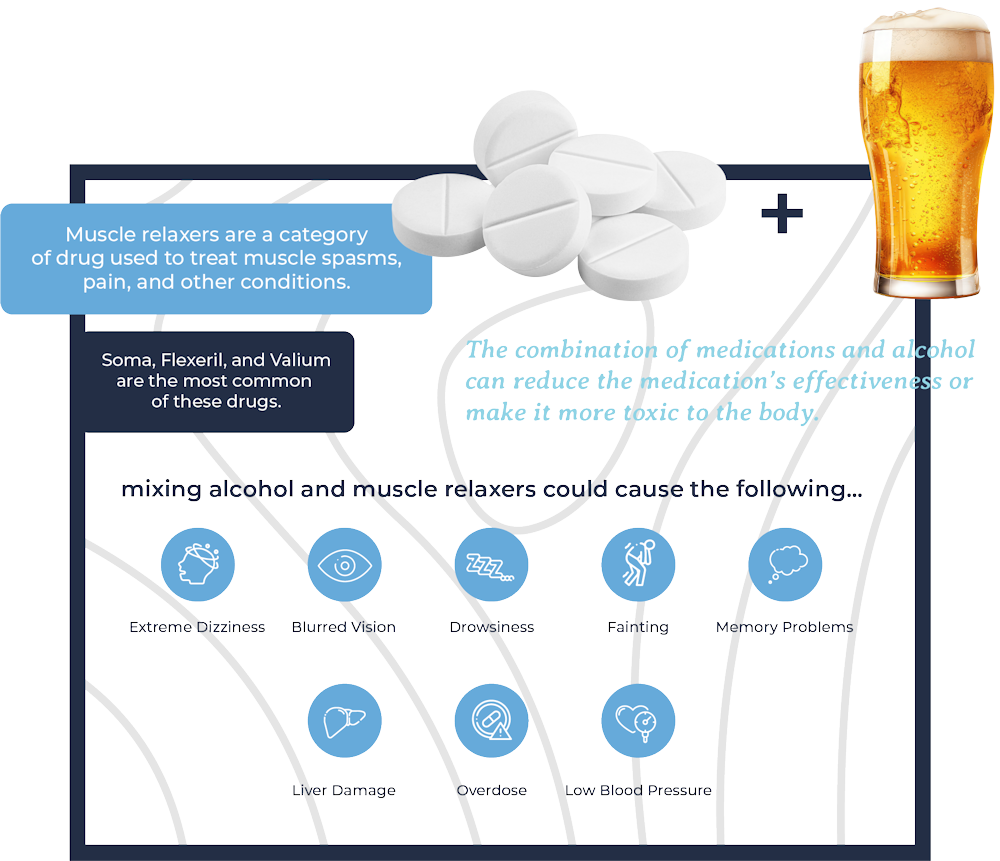
The combination of drugs with alcohol, especially in the case of muscle relaxers, is strongly discouraged. Since alcohol is itself classified as a drug, this mixture falls under both drug-beverage interactions and drug-drug reactions.
For those seeking assistance with alcohol or prescription drug-related concerns, our team at Crestview Recovery in Portland provides comprehensive alcohol rehab and prescription drug rehab services.
What are Muscle Relaxers?
Muscle relaxers are a category of drug used to treat muscle spasticity, pain, and other conditions. Muscle spasms are the involuntary and sudden contractions of a muscle or group of muscles that are usually accompanied by severe pain. Many things can cause muscles to start acting up, such as fibromyalgia, neck pain, and lower back pain.
There are many types of muscle relaxers and they all have their unique ways of working. Carisoprodol (Soma), cyclobenzaprine (Flexeril), and diazepam (Valium) are probably the most common and well-known of these drugs.
What Do Muscle Relaxers Do?
The various kinds and brands of skeletal muscle relaxers react differently to alter muscle function. Almost all muscle relaxants have a sedative effect and focus their effects directly onto the central nervous system and nerve pathways that send signals of pain and pleasure to and from the brain.
Generally, antispastic medications directly act on your skeletal muscle or spinal cord to improve involuntary spasms and muscle tightness (hypertonicity).
Antispasmodics use the central nervous system to change signals in your brain and spinal cord to decrease muscle spasms.
What Conditions are These Prescribed for?
Antispastics and antispasmodics have specific and different uses, though they are both types of skeletal muscle relaxants. Some of these medications are used to treat conditions that are not related to muscle function, such as diazepam being used to treat anxiety in Portland and seizures. There are two main types of muscle relaxants used in treatments, namely antispastic medication and antispasmodic medication.
Antispastic Medication
Spasticity is defined as a disturbance in muscle movement patterns that causes specific muscles to contract all at once whether someone is moving around or completely at rest. This is usually a result of damaged nerve pathways inside the spinal cord or brain that regulate stretch reflexes and movement.
Several conditions that can lead to spasticity are:
- Cerebral palsy
- Multiple sclerosis (MS)
- Spinal cord injury
- Stroke
- Brain or head injury
- Amyotrophic lateral sclerosis (ALS), (Lou Gehrig’s disease)
Antispasmodic Medication
Musculoskeletal and myofascial pain (notably lower back pain) and muscle spasms are what antispasmodic skeletal muscle relaxants are normally prescribed for.
These medications are usually used as an alternative, last-resort treatment after first-line medications haven’t worked. This is mainly because of the addiction potential and other side effects of antispasmodic drugs.
How Common are Muscle Relaxers?
The frequency of chronic and acute back pain makes muscle relaxants a relatively common prescription. Lower back pain is one of the top five reasons people see their primary healthcare providers. Most cases resolve themselves naturally, but severe cases may be prescribed a muscle relaxant.
Due to their potential to develop addictions diazepam and carisoprodol are usually only prescribed for short periods. Other prescription muscle relaxants do not create addictions.
What are the Side Effects of Muscle Relaxers?
The various prescription muscle relaxants all have different possible side effects. Speak with your primary caregiver about the possible side effects of the specific medication you’re on or considering taking.
A few general side effects of muscle relaxants include:
- Drowsiness and fatigue
- Dizziness
- Nausea
- Headache
- Dry mouth
- Fainting and blurred vision
Do Muscle Relaxers Make You Sleepy?
Yes. Prescription muscle relaxers are depressants and affect the central nervous system in ways that make you drowsy. Try not to operate heavy machinery, drive, or make important decisions while under the influence of these medications.
Are Muscle Relaxers Addictive?
Diazepam and carisoprodol are regulated substances, meaning that they have the potential to create addictions and can cause withdrawal symptoms if a patient develops a dependence on them and stops taking them suddenly. If you have a family history of substance use disorders, you should try to avoid these medications.
If you are on either of these medications and feel that they aren’t effective or that you’re becoming dependent, do not take more than your recommended dosage. Speak to your healthcare provider immediately, or reach out to your nearest treatment center.
Can You Overdose on Muscle Relaxers?

Certain muscle relaxers, such as Diazepam and carisoprodol, have the potential to be abused and create addictions. Prolonged use can increase physical dependence and tolerance. Knowing what prescription drug misuse is and what it looks like can help identify a problem such as dependence before it goes too far.
Most muscle relaxers are sedatives, and some people combine them with other drugs for nonmedical reasons to induce or enhance feelings of dissociation and euphoria.
The misuse of muscle relaxers can cause an overdose which can lead to:
- Changes in consciousness
- Hallucinations
- Seizures
- Respiratory depression
- Cardiac arrest
- Coma
- Death
Should You Drink While Taking Medication?
Drinking alcohol while taking medication is risky and should be avoided. The combination of medications and alcohol can reduce the medication’s effectiveness or make it more toxic to the body.
Prescription muscle relaxers and alcohol should never be mixed. Both muscle relaxers and alcohol are depressants, meaning they slow down the body’s central nervous system. Mixing them could cause the following dangerous side effects:
- Extreme dizziness
- Extreme drowsiness
- Blurred vision
- Low blood pressure
- Fainting
- Memory problems
- Liver damage
- Increased risk of overdose
What Can Happen When You Drink While Taking Medication?
Alcohol and medication are a deadly combination. Alcohol reacts with hundreds of prescription and over-the-counter medications to cause serious damage to the body and mind.
A few consequences of drinking alcohol while taking medication are:
- Nausea and vomiting: Certain medications, such as chemo drugs, cause nausea and vomiting, especially when taken on an empty stomach. Combining these medications with alcohol can increase the nausea effect and make you vomit excessively enough to lose fluids and electrolytes.
- Headaches: Surprisingly, drinking copious amounts of alcohol can make you dehydrated, and dehydration causes painful headaches. Medications like antibiotics, antidepressants, and blood pressure drugs also have ‘headaches’ as a possible side-effect, and when combined with alcohol can cause migraines or other severe headaches that are hard to get rid of… without taking more medication.
- Drowsiness: Medications like antihistamines, painkillers, and anxiety drugs often make you sleepy. When combined with alcohol these medications can increase the risk of you nodding off at the wrong place and time, like behind the wheel or in the pool.
- Fainting: Alcohol can lower blood pressure, and when combined with diuretics, beta-blockers, nitrates, and other medications can make you lightheaded and dizzy enough to pass out and injure yourself.
- Shifts in blood pressure: Depending on how much and how often you drink alcohol, your blood pressure could become irregular. This effect is magnified if you add medications such as calcium channel blockers, angiotensin-converting enzyme (ACE) inhibitors, and angiotensin receptor blockers (ARBs). This combination can make your blood pressure spike too high or reduce it low enough to induce strokes or other heart problems.
- Abnormal behavior: Alcohol acts on the brain receptors that control moods and emotions, which can make you more aggressive or lead you into a pit of anxiety and depression. Combining alcohol with medications such as mood stabilizers, antidepressants, and antipsychotics increases the likelihood of violent outbursts and unpredictable behavior.
- Loss of coordination: Alcohol impairs reflexes and motor skills, making you slow and clumsy. Muscle relaxers, anticonvulsants, and sedatives also impair the body’s mobility, and when combined with alcohol can be fatal.
- Internal bleeding. Excessive consumption of alcohol can result in damage to the stomach’s lining as well as ulcers or bleeding. Medications containing blood-thinning components, such as aspirin, ibuprofen, naproxen, warfarin, and clopidogrel, when combined with alcohol, increase the risk of internal hemorrhaging and bleeding that may be life-threatening.
- Impaired breathing: Alcohol can reduce your breathing rate and depress your central nervous system. Some medications can do the same, such as opioids, sleep aids, benzodiazepines, and barbiturates, so mixing the two increases the risk of respiratory failure or death.
- Liver damage. Alcohol can cause scarring, inflammation, and other permanent deterioration of your liver. Certain medications, if abused, can also affect your liver’s normal functioning or damage it, such as acetaminophen (Tylenol), antibiotics (such as erythromycin), statins (cholesterol-lowering drugs), antifungals (such as ketoconazole), antivirals (such as ritonavir), antituberculosis drugs (such as isoniazid), amiodarone (a heart drug), anticonvulsants (such as valproic acid), methotrexate (a cancer drug), etc. Combining alcohol and medication is a recipe for disaster for your liver.
Hospitalization or death is not worth the risk of drinking while you take medication. You may think that you can handle it, or that nothing will happen, but you won’t know how alcohol will react with your medication until it’s too late. If alcohol use is a concern for you, alcohol rehab in Portland can help address the underlying causes of why you drink and help you become sober.
How Long Should You Wait to Drink After Taking a Muscle Relaxer?

Your weight, liver function, age, and other factors all determine the length of time you should wait before drinking alcohol after taking muscle relaxers. Muscle relaxers generally remain in the system for longer than 24 hours, so to be safe, wait at least 36 hours before drinking any alcoholic beverages. If you absolutely must drink within that period, drink much less than your usual amount, and do not drive or operate machinery.
Treatment for Alcohol and Prescription Drug Addiction at Crestview Recovery
While prescription medication is there to help us through tough times, both physically and mentally, there always remains the potential to become addicted. Building up a tolerance to alcohol and/or medication does happen, and you should never feel ashamed about seeking help to cut the addictions and dependencies.
If you or a loved one are struggling with alcohol use disorder or substance use, help is available for you at Crestview Recovery. Our wide range of addiction treatment programs in Oregon includes residential treatment, outpatient treatment, skill-building, counseling, and much more. Our experienced and professional team will work with you to build a recovery program that caters exclusively to your needs and preferences. Contact us today to speak with our admissions personnel about enrollment, or schedule a visit to experience what we have to offer firsthand.